Aroma-oral care pilot study (hydrolats) 🤓
Objectives: An aroma-oral care pilot study was conducted to explore the effects of aromatic water that was added to regular oral hygiene care in palliative patients.
Design: Aromatic water mixture (AWM) was added to regular oral hygiene care in palliative patients at five different Slovenian care facilities. Each staff member using the protocol filled out a questionnaire, wrote up case studies and made a review of the results.
Methods: AWM was added to regular oral hygiene care by replacing the regular solution used in mechanical oral care or as an addition to regular oral care as a daily spray. The original AWM consisted of equal parts of the hydrolats of Satureja montana (winter savory), Laurus nobilis (laurel leaf) and Salvia officinalis (sage). In 11 cases, participants chose to use a different hydrolat or hydrolat mixture instead.
Results: 24 palliative patients participated in this study. 75% of patients had better mouth odour and reported that the oral mucosa was more hydrated, 70% of patients had less coating in the mouth and a better tongue colour. There were no contraindications and 100% reported satisfaction from the staff using the hydrolats.
Conclusion: The study results showed that incorporating hydrolats in oral hygiene can help refresh oral mucous membranes, improve breath odour, taste and other aspects of oral care. This gentle and affordable addition to regular oral care has no negative side effects and provides a broad spectrum of potential benefits that should be further explored.
Introduction
Oral hygiene is an important aspect of a healthy life. With appropriate oral hygiene, we can significantly influence quality of life. With ageing and disease, our body is subjected to social, mental and physical changes. Due to changes in lifestyle, the oral cavity also manifests changes that may consequently result in disorders in metabolism and nutrition. Besides degenerative changes in connective tissue, atrophy of epithelium and bone are also frequent (Rode, 2008). Physiologically, reduction of the secretion of saliva is a risk factor for the development of conditions in the oral cavity such as dry mouth, mouth ulcers, fungal infections (such as Candida albicans), coating/ plaques in the mouth, periodontal disease, and decreased quality of life (Locker et al, 2002). A damaged/ fragile oral mucosa creates an environment suitable for developing various infections. It is also related to sleep disturbances, poor nutrition, and even communicational and cognitive degeneration (Villanueva-Vilchis et al, 2016). The primary goal of our pilot study was to assess beneficial effects of hydrolats and their blends in addressing abovementioned symptoms by providing palliative care patients with AWM solution alongside their regular oral hygiene procedures two to five times per day.
Materials and Methods
The main goal of the aroma-oral care study was to increase the effectiveness of oral hygiene by introducing aromatic waters/ hydrolats. Other specific study goals included addressing symptoms such as dry mouth, foul breath, soreness and inflammation in the mouth, as well as stimulating the appetite.
The study was conducted across five different facilities in Slovenia:
- Home for elderly care DEOS, Center starejsih Crnuce represented by Petra Jenko, Occupa- tional Therapist.
- Home for elderly care DEOS, Center starejsih Zimzelen Topolica represented by Andreja Stefan Bukovic, Director of the Care Center of Elderly and Ana Simenc, Working Instructor.
- Home for elderly care Dom Petra Uzarja, rep- resented by Maja Krzisnik, Registered Nurse.
- Home for elderly care Logatec represented by Mojca Tuljak, Occupational Therapist.
- General Hospital Jesenice, Center for interdisciplinary pain treatment and palliative care, Mobile palliative team represented by Darja Noc, Registered Nurse.
All the listed facilities added aromatic water mixture (AWM), described below, to their daily oral care routine to between three and six of their patients.
Eleven AWMs were modified during the study to meet patients’ specific requirements.
The aromatic water mixture of Satureja montana (winter savory), Laurus nobilis (laurel leaf) and Salvia officinalis (sage) hydrolats in equal parts was provided to palliative patients two to five times a day for a minimum period of three days and a maximum period of 145 days with an average of 48 days. An overview of the time period is presented in Figure 1.
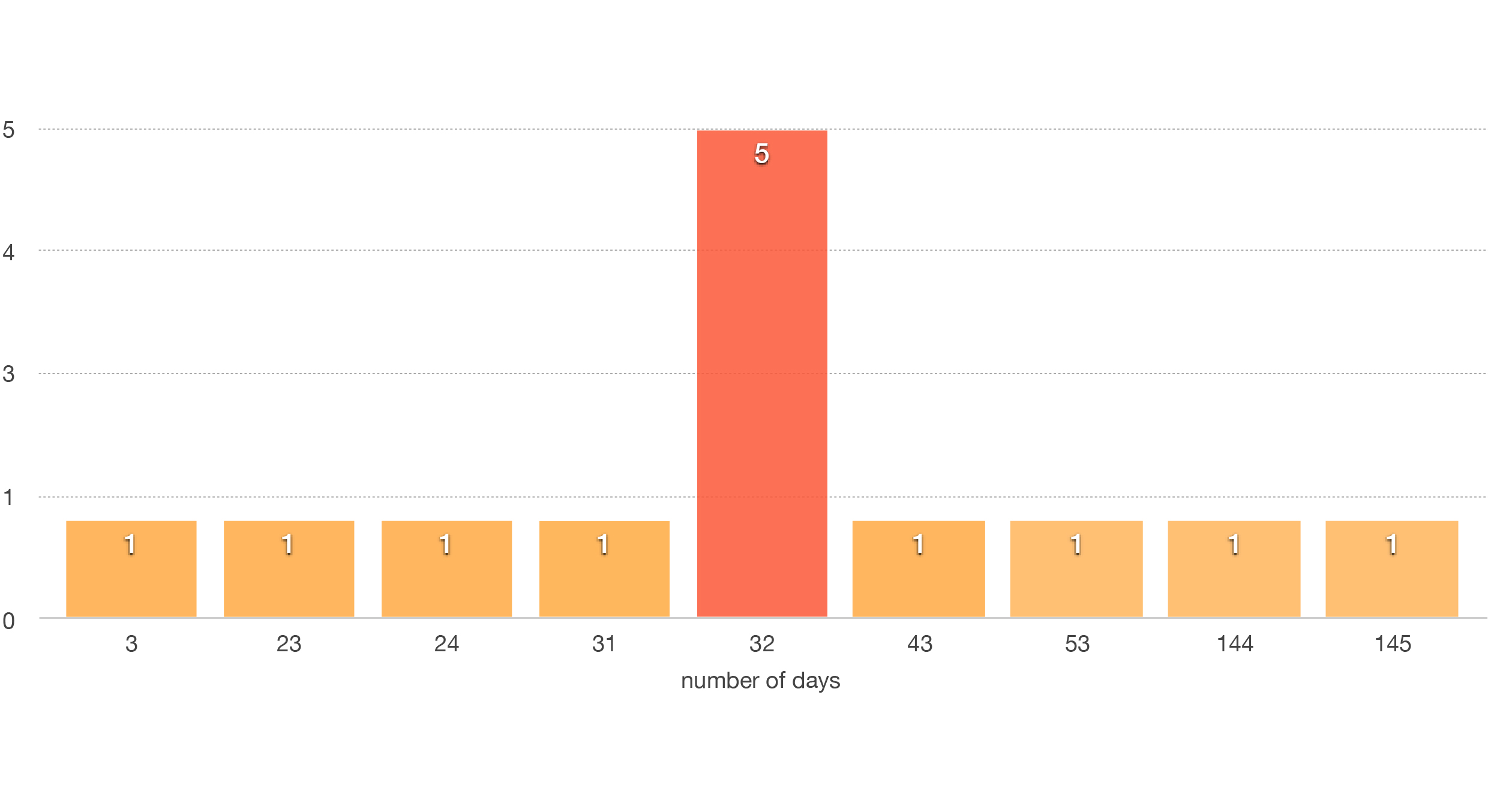
Figure 1. Overview of number of days using only the original AWM together with patient numbers.

The hydrolats were selected for their properties as well as the fact that they are from herbs that are commonly used and thus familiar in Slovenia. The taste and smell of the mixture may thus remind patients of familiar food, home and comfort.
Additional motivation for selecting locally produced hydrolats was to support local distillers and to use hydrolats that are as fresh as possible. Local distillers donated hydrolats used in the study.
Table 1 provides more details about the selected hydrolats and the rationale for their selection.
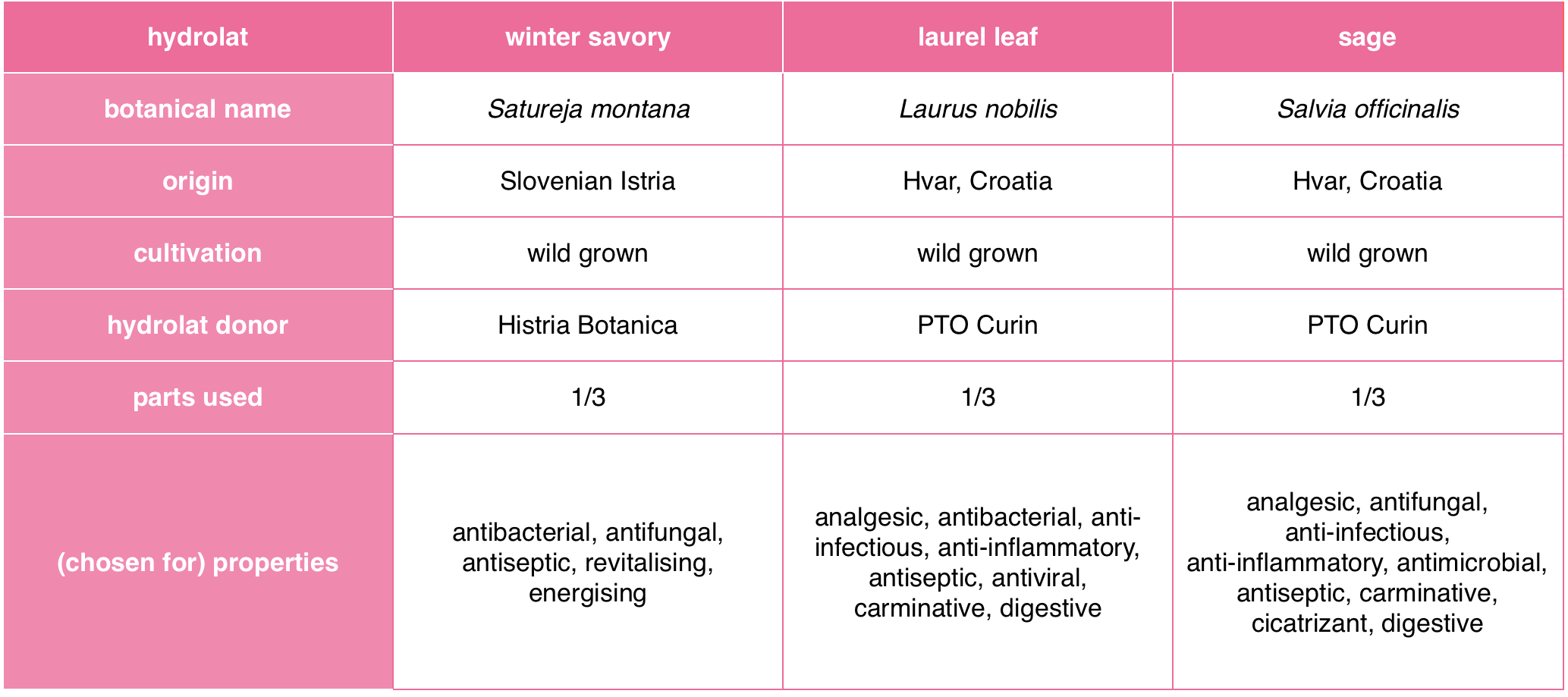
Satureja montana hydrolat was selected for its antibacterial, antifungal, antiseptic (Catty, 2001), revitalising and energising (Price and Price, 2004) properties.
Laurus nobilis was chosen for its analgesic, anti-infectious, anti-inflammatory (Price and Price, 2004), antiseptic, antibacterial, antiviral (Harman, 2015), carminative and digestive (Price and Price, 2004; Rose, 1999) properties.
Salvia officinalis was chosen for its analgesic, antifungal, antimicrobial, carminative (Harman 2015), anti-infectious, anti-inflammatory, antiseptic, cicatrisant and digestive properties (Price and Price, 2004).
The hydrolats were wild grown and locally sourced.

The still, plant and field photos are provided by one of the hydrolat donators – Bonistra.
Method one: AWM sprayed onto oral care sponges and used to clean the oral cavity twice a day, in the morning and evening.
Method two: AWM sprayed into the mouth after regular oral care and additionally during the day (three to five times a day).
In total, 24 elderly patients (12 male, 12 female) participated in the study. The age of the patients ranged from age 46 to 95 with an average age of 74 years. All patients are in the palliative care stage.
Thirteen (4 male, 9 female) used the original AWM, 10 of which added AWM to their daily oral care routine twice a day (first method) and the other three participants applied AWM three to five times a day (second method). Two patients chose an aromatic water mixture of winter savory and laurel leaf in equal parts applied via the first method instead of the original AWM. Seven patients chose a single winter savory hydrolat and two chose sage hydrolat alone.
More detail is provided in Figure 2.
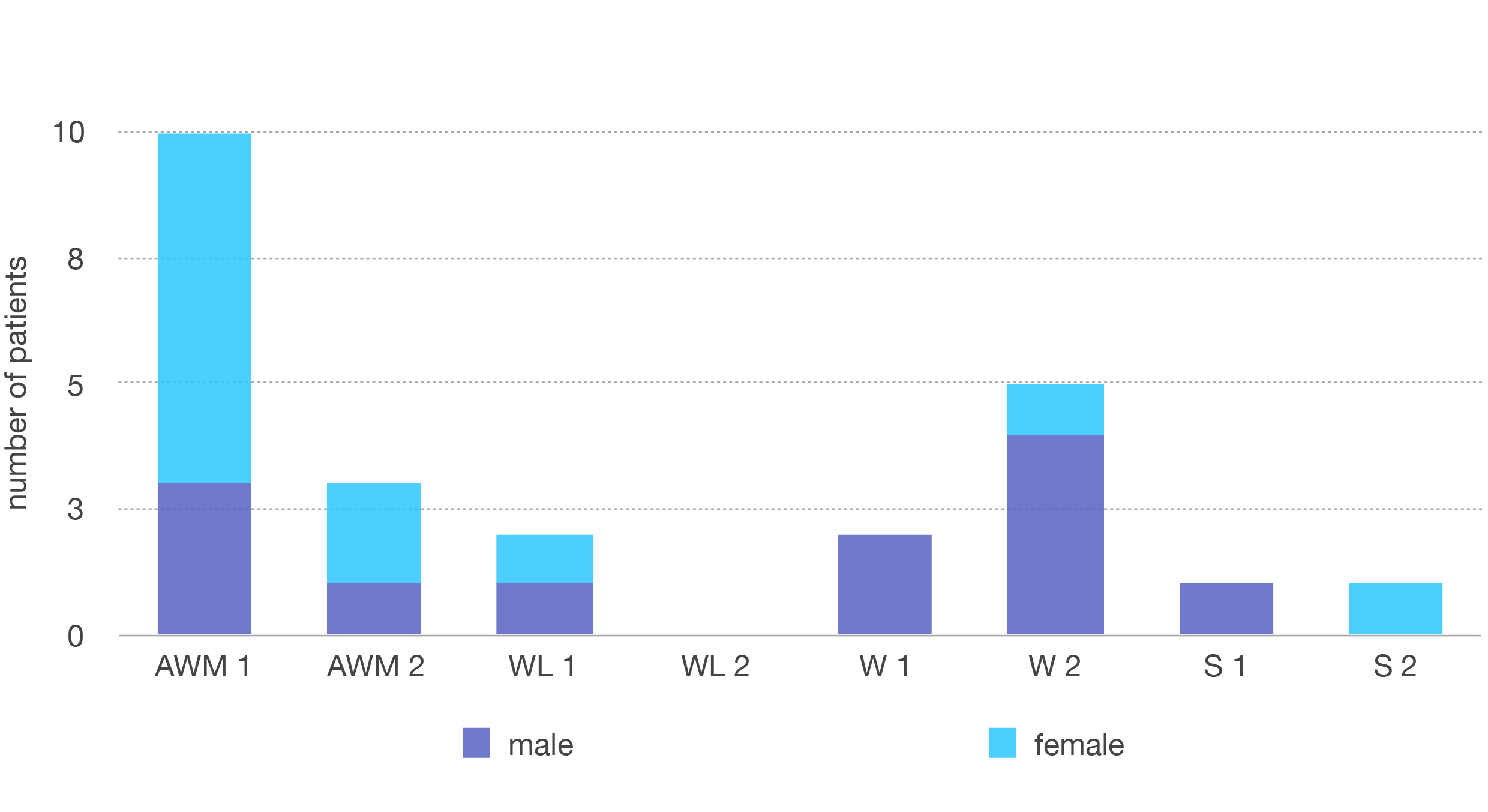
Figure 2. Total number of patients who completed the study.
Legend:
AWM1 – original AWM using the first method
AWM2 – original AWM using the second method
WL1 – aromatic water mixture of winter savory and laurel leaf using the first method
WL2 – aromatic water mixture of winter savory and laurel leaf using the second method
W1 – winter savory hydrolat alone using the first method
W2 – winter savory hydrolat alone using the second method
S1 – sage hydrolat alone using the first method
S2 – sage hydrolat alone using the second method
General oral concerns of the patients included: dry mouth and mouth mucosa, foul breath and taste, coating in the mouth, poor tongue colour, bleeding gums and lips, mouth ulcers, difficulty swallowing, pain and inflammation in the mouth, oral candidiasis, poor appetite. All 24 patients had dry oral mucosa, foul breath, a coated mouth and poor tongue colour.
To examine the effect of hydrolats after application, the medical staff supervising the patients wrote case studies and follow up reports as well as completing a qualitative questionnaire at the end of the monitoring period. The questionnaire included qualitative results on mouth mucosa, foul breath, mouth coating and tongue colour. If the medical staff noticed other relevant concerns such as bad taste in the mouth, mouth ulcers, pain and inflammation in the mouth at the beginning of monitoring period, those were also graded and included in the report as.
Patients’ preferences to the taste and smell were categorised into following categories:
- likes it
- reminds of food
- got used to it
- dislikes it
- no reaction
The medical staff monitoring the patients reported any contraindications as well as unpredicted results, concerns, comments and expressed their satisfaction/dissatisfaction with the results. The analysis was then made based on the reported scores.


Figure 3. Photos: Results for one patient before [left] and after [right] use of the original AWM.
Reproduced with permission from Petra Jenko, Home for Elderly Care DEOS, Center Starejših Črnuče.
https://www.deos.si/crnuce
Results
Results using the original AWM
The most significant effects of complementing regular oral care in palliative patients with the selected AWM were concerning coating of the mouth and tongue colour. 12 out of 13 patients (92%) had less mouth coating and better tongue colour as shown in the photos (before and after).
The next significant difference was concerning foul breath. Nine out of 13 patients (69%) experienced noticeably better breath odour and in five cases (38%), their halitosis has completely disappeared.
Additional results were that five out of 13 (38%) reported good results in resolving dry mouth and seven of 13 (53%) reported that their oral mucosa was more hydrated.
I would like to point out here, that one facility (i.e. six out of 13 study participants) omitted to report the results regarding monitoring the level of mucosal moisture – this accounts for the lower level overall of AWMs’ effectiveness than expected.
Other facilities (i.e. seven study participants) reported an increased level of moist mucosa as one of their most significant results.
Other relevant improvements the medical staff noticed include fewer mouth ulcers (three cases), less inflammation in the mouth (three cases), reduction of Candida albicans (one case) and in one case the bleeding of the gums and mouth stopped completely.
With regards to the taste of the hydrolats, eight out of 13 (62%) patients liked the original AWM, ne disliked it, three got used to it and one had no reaction. We did not observe any significant changes in appetite or taste. Furthermore, eight patients liked the smell of original AWM, four had no reaction and two were unable to communicate.

Results using other hydrolats
As previously mentioned, in cases where patients disliked the taste or the smell of the AWM, a more individualised approach was used. 11 patients tested Satureja montana (winter savory), Laurus nobilis (laurel leaf) and Salvia officinalis (sage) hydrolat separately and chose the one that they liked the most. Two patients chose an aromatic water mixture of winter savory and laurel leaf in equal parts; seven patients chose a single winter savory hydrolat and two chose sage hydrolat alone.
For the two patients who used an aromatic water mixture of winter savory and laurel leaf hydrolats in equal parts, both had better breath odour, a more hydrated oral mucosa and resolved dry mouth. Less coating in the mouth and better tongue colour in addition to better taste and less gum sensitivity was reported at one out of two cases. One patient liked the smell and the taste; it reminded her of home, the other did not like the taste or smell at first but got used to it.
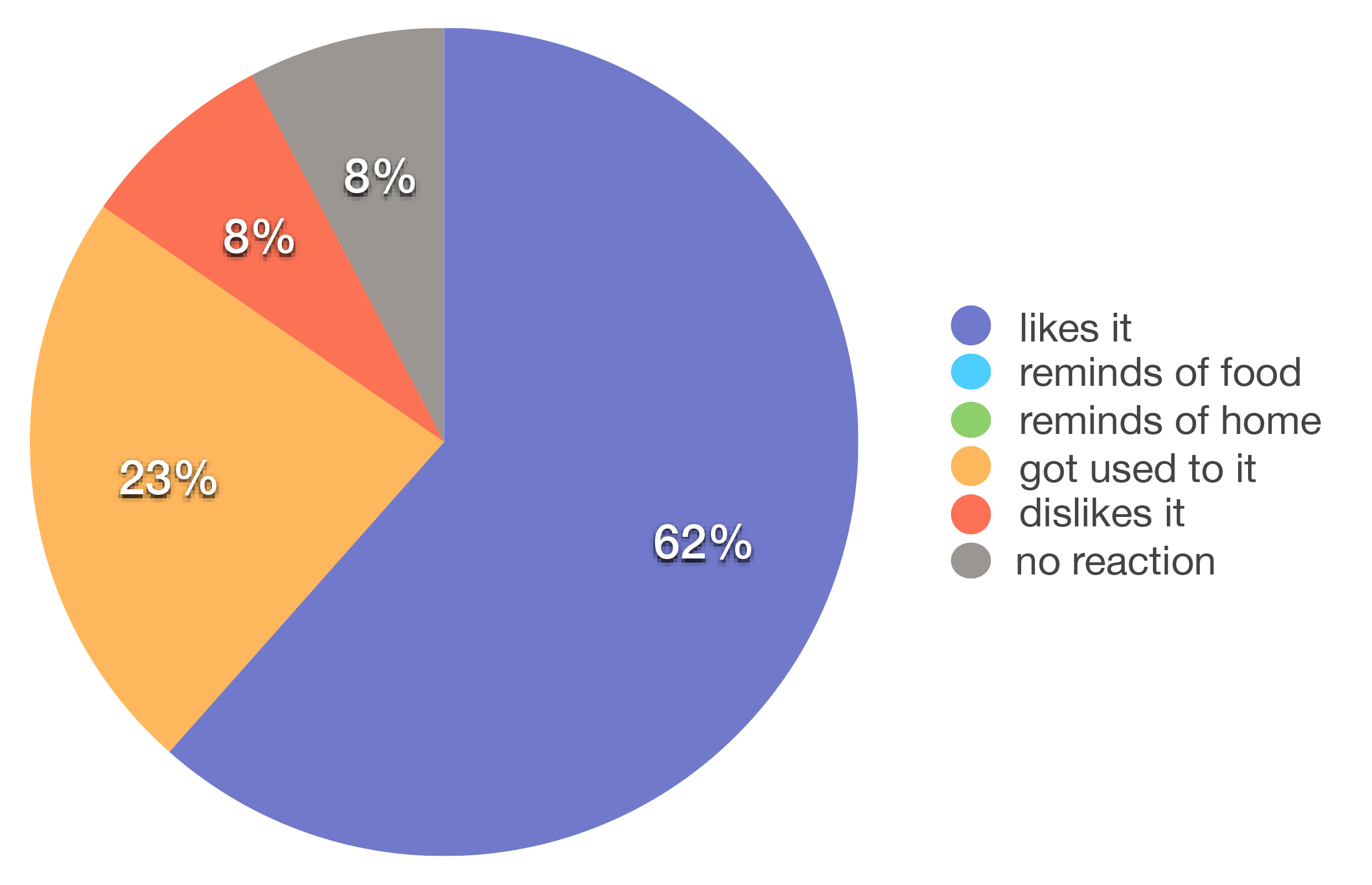
Fig 5. Taste assessment review using the original AWM.
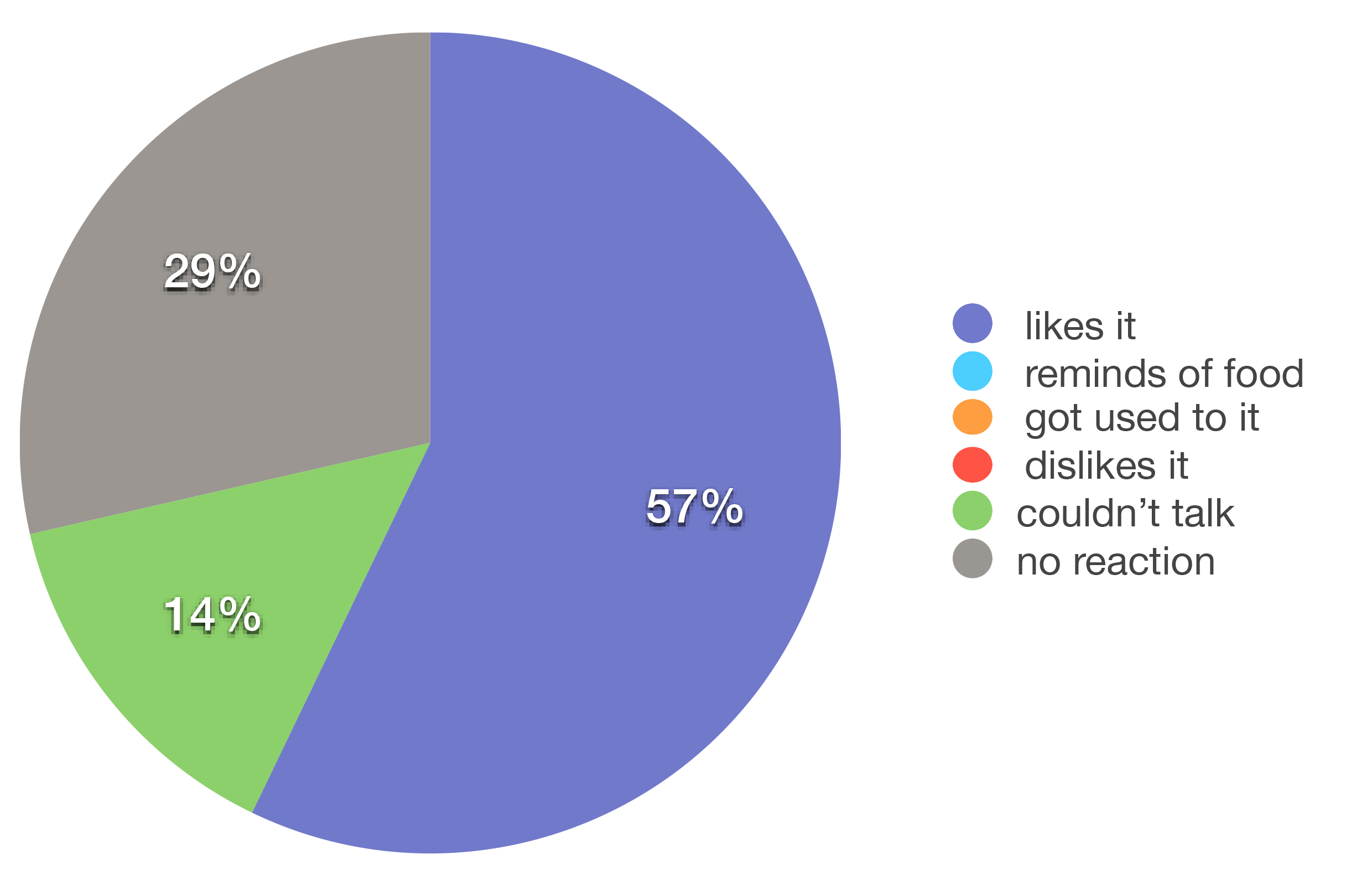
Fig 6. Smell assessment review using the original AWM.
For the seven patients who used winter savory hydrolat alone, the best results were a more hydrated oral mucosa (100 %), followed by better breath odour and resolved dry mouth (71%: five out of seven) and less mouth coating (42%: three out of seven).
Other relative results include less pain and inflammation in the mouth in three out of seven cases and fewer mouth ulcers in two cases.
Six out of seven patients liked the smell and taste, three reported it reminded them of food as well and one patient didn’t like it at first but got used to it.
For the two patients who chose sage hydrolat on its own, both experienced less inflammation in the mouth, had better breath and a more hydrated oral mucosa. There was less coating in the mouth and a better tongue colour as well as resolved dry mouth, better taste, less pain and redness in the throat in one out of two patients. Both patients liked the smell and the taste.
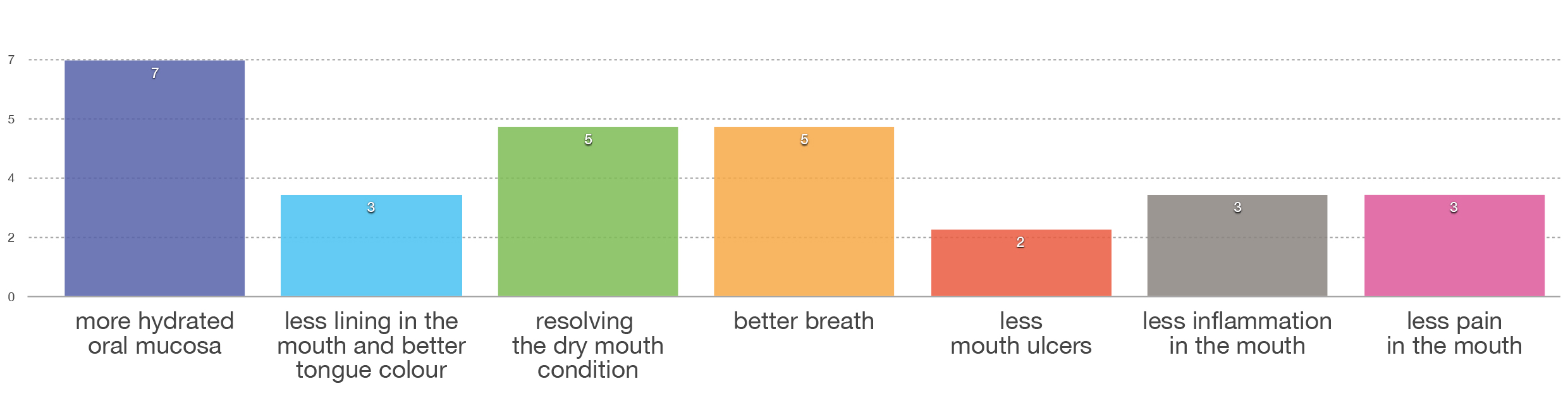
Figure 7. Overview of results using winter savory hydrolat alone.
Staff satisfaction
There were no negative results and/or contra- indications and 100% satisfaction with the results from the staff using the hydrolats. Some comments from nurses and therapists are included here:
“We are pleased with the results from the study. Next time, we should take more time to test individual hydrolat preferences for each patient. That way we could achieve fewer rejections and be more successful. The great thing about AWM is that it is natural and less aggressive than the usual cleaning solutions used. AWM taste is particular and might not be for everyone, at least not at the beginning. Some patients need time to get used to it.”
Mojca Tuljak, Home for elderly care Logatec
“I am very pleased with the results in the cases that I have monitored. When I talked to the patients and explained to them what we wanted to achieve, they were excited. In cases where the study was carried out by an uneducated staff member, the results were not as good. My findings are that basic aromatherapy knowledge is necessary for better results. I will continue to use AWM for hydrating mouth mucosa in my work as well as in my private life.”
Darja Noc, General Hospital Jesenice
“Due to our success with AWM, we started using Helichrysum italicum (everlasting) hydrolat for skin care in our Center and have amazing results. Our staff, patients and patients caregivers are thrilled with the positive results. We will continue using hydrolats in our work and studies.”
Petra Jenko, Home for elderly care DEOS, Center starejsih Crnuce
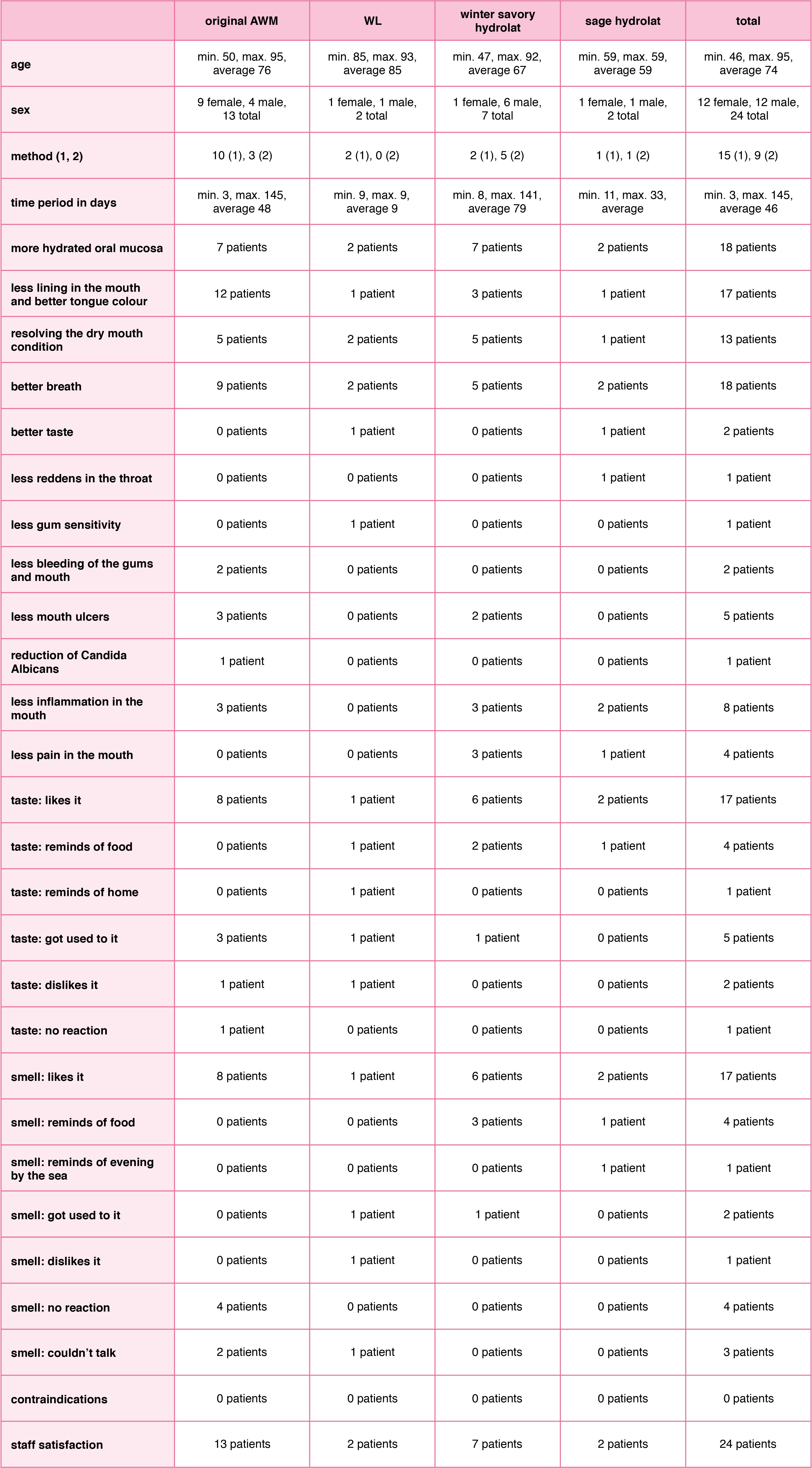
Table 2. Overall summary of study results
Individual case study examples
The most significant effects of complementing regular oral care in palliative patients with the selected AWM were concerning coating of the mouth and tongue colour. 12 out of 13 patients (92%) had less mouth coating and better tongue colour as shown in the photos (before and after).
AWM oral care case study
An 82 year old female patient in terminal palliative care had oral candidiasis, dry oral mucosa and has a nasogastric tube.
Our goal was to refresh and improve oral cavity.
We cleaned the oral cavity with the original AWM twice a day: in the morning at 8 am and evening at 7 pm. AWM was sprayed onto oral care sponges – these were used to clean the oral cavity. One sponge was used for the upper gums then a new one to clean all of them, and a third one to clean the tongue. More sponges were used if necessary.
The intervention started on February 6th, 2017 and we continue to use it (report written on March 31st, 2017).
The results included:
- less coating of the mouth and better tongue colour (score 8/10)
- Candida albicans decreased but not completely resolved (score 8/10)
- less dryness in the mouth (score 10/10)
- less inflammation (score 8/10).
The patient cannot speak but nods her head to confirm that she likes the taste and smell. When using AWM, the patient looks satisfied and relaxed. We are pleased with the results. I would suggest using it more frequently for better results.
AWM spray case study
A 79-year-old female patient in palliative care had bleeding gums and lips as well as mouth ulcers. Our goal was to improve the condition of the oral mucous membrane, so that routine oral care would not be as painful.
We used AWM spray three times a day (or more) from November 23rd, 2016 to January 18th 2017, when she passed away. The patient liked the taste and had no reaction to the smell.
The results included a more hydrated mucosa (score 7/10), as well as less coating in the mouth, less bleeding and mouth ulcers. The tongue was not as white anymore and the breath odour improved. The patient, her caregivers and the staff were all pleased with the results.

Satureja montana (winter savory) case study
A 61-year-old male patient in palliative care with throat cancer has trouble swallowing and burning pain in the mouth with constantly dry mouth mucosa and poor appetite. He was nervous and irritable. He has a tracheostomy and talks with a speaking device. Our goal was to refresh his oral mucous membrane as well as improve taste and breath odour.
We used winter savory hydrolat spray three to five times a day. During the day, the patient used a 30ml winter savory hydrolat spray when he felt he needed refreshment. The intervention started in March 2017 and we continue to use it today (report written on April 25th, 2017).
The results included:
- less lining the mouth and better tongue colour (score 5/10)
- fewer mouth ulcers (score 6/10)
- less dryness in the mouth (score 8/10)
- better breath (score 8/10)
- less pain (score 6/10)
- less inflammation (score 4/10)
- better taste (score 8/10).
The patient likes the taste as well as the smell and it reminds him of food. The patient reports that:
- he enjoys his winter savory hydrolat spray very much
- has a pleasant sensation in the mouth
- has less “burning” pain
- has less oral thrush
- has better taste
- and better breath.
We met our goal. The patient is in a better mood, his mouth mucosa is moist and less painful. He asked for a winter savory hydrolat spray refill for the third time.
Salvia officinalis (sage) case study
A 59-year-old female with pancreatic cancer in palliative care. She is in her third and fourth chemotherapy cycle phase. She is weak and in a poor mood with occasional insomnia. She has a foul breath, especially in the morning. She wakes up with sticky mouth and lips. She has poor appetite and doesn’t eat the food she had previously enjoyed. Our goal was to refresh oral mucous membrane, improve taste and mood of the patient.
We used sage hydrolat spray three to five times a day. In the morning, she brushed her teeth as usual and used the sage hydrolat spray during the day to hydrate the oral mucosa. The intervention started in March 2017 and we continue to use it (report written on April 25th, 2017).
The results include:
- less lining the mouth and better tongue colour (score 8/10)
- less dryness in the mouth (score 8/10)
- better breath (score 8/10)
- less inflammation (score 3/10)
- better taste (score 8/10).
The patient likes the taste as well as the smell of the hydrolat and it reminds her of food and evenings by the sea. The patient reports that she especially enjoys using the spray just before she goes to sleep because she wakes up with a completely different (better) feeling in the mouth than when she is not using the spray. Her mouth doesn’t feel uncomfortable and she no longer has sticky lips and mouth. She is also less thirsty.We are pleased with the results and the patient will continue using sage hydrolat spray for hydrating her oral mucosa.
Conclusion
In the present pilot study, aroma-oral care was performed on senior patients in palliative care and was found to improve mouth mucosa, foul breath, dry mouth, mouth coating and tongue colour.
In addition, improvement was reported in mouth ulcers, pain and inflammation.
A patient’s choice of the hydrolat used in their care seemed to play an important role with regards to obtaining more successful results. Nevertheless, 62% of patients liked the taste and smell of the original AWM. Medical staff reported better results and improved patient cooperation when a more individualised approach was used regarding the choice of hydrolats for oral care.
Limitations of the present study include a low patient number, two methods of application as well as a limited questionnaire due to unforeseen relevant information. In future studies, a greater number of patients may need to be evaluated for every method of application separately to clearly demonstrate the effect of aroma-oral care on senior patients in palliative care. Studies on patients with mouth ulcers, pain and inflammation need to be further explored as well.
Moreover, using hydrolats in oral hygiene has no negative results and/or contraindications and 100% satisfaction with the results.
The study results show that incorporating hydrolats into regular oral hygiene can help refresh oral mucous membranes, improve breath, taste and other aspects of oral care. This gentle and affordable addition to regular oral care has no negative side effects and provides a broad spectrum of potential benefits that should be further explored.
Acknowledgments
Andreja Stefan Bukovic, Ana Simenc, Darja Noc, Maja Krzisnik, Mojca Tuljak and Petra Jenko for their research and cooperation with this study. Stjepko Curin (PTO Curin), Jana Bergant (Bonistra) for donating hydrolats and Petra Sedej (Aromazen) for donating spray bottles. Maja Pecenic for her advice in the writing of this article.
References
Catty, S. Hydrosols: The Next Aromatherapy. Vermont: Healing Arts Press; 2001.
Harman, A. Harvest to Hydrosol : Distill Your Own Exquisite Hydrosols at Home. USA: botANNicals; 2015.
Microbiol Infect Dis, 32:1311-1320.
Price L, Price S. (2004) Understanding Hydrolats: The Specific Hydrosols for Aromatherapy: A Guide for Health Professionals. Churchill Livingstone; 2004.
Rode M. Ustna votlina v starosti. Zdrav Vestn. 2008;77:839-
845. Locker D, Matear D, Stephens M, Jokovic A. Oral
health-related quality of life of a population of medically compromised elderly people. Community Dent Health. 2002; 19(2):90-97.
Manczinger M, Bocsik A, Kocsis GF, Vörös A, Hegedűs Z, Ördögh L, Kondorosi É, Marton A, Vízler C, Tubak V, Deli M, Kemény L, Nagy I, Lakatos L (2015). The absence of N-Acetyl-D-glucosamine causes attenuation of virulence of Candida albicans upon interaction with vaginal epithelial cells in vitro. Biomed Res Int, Article ID:398045.
Mar Rodríguez M, Pérez D, Javier Chaves F, Esteve E, Marin-Garcia P, Xifra G, Vendrell J, Jové M, Pamplona R, Ricart W, Portero-Otin M, Chacón MR, Fernández Real JM (2015). Obesity changes the human gut mycobiome. Sci Rep, 5:14600.
Maruyama N (2007). Aromatherapy care for oropharyngeal candidiasis based on scientific research. IJCA, 4(2):3-9.
Metchnikoff É (1908). The Prolongation of Life: Optimistic Studies (trans ed, Chalmers Mitchell P). Internet Archive. https://archive.org/details/prolongationofli00metciala
Ninomiya K, Hayama K, Ishijima SA, Maruyama N, Irie H, Kurihara J, Abe S (2013). Suppression of inflammatory reactions by terpinen-4-ol, a main constituent of tea tree oil, in a murine model of oral candidiasis and its suppressive activity to cytokine production of macrophages in vitro. Biol Pharm Bull, 36(5):838-844.
Ninomiya K, Hayama K, Ishijima S, Takahashi M, Kurihara J, Abe S (2013). Effects of inhibitory activity on mycelial growth of Candida albicans and therapy for murine oral candidiasis by the combined use of terpinen-4-ol and a middle-chain fatty acid, capric acid. Yakugaku Zasshi, 133(1):133-140. In Japanese.
Pinto E, Hrimpeng K, Loped G, Vaz S, Gonçalves MJ, Cavaleiro C, Salgueiro L (2013). Antifungal activity of Ferulago capillaris essential oil against Candida, Cryptococcus, Aspergillus and dermatophyte species. Eur J
Rose, J. 375 Essential Oils and Hydrosols. Berkeley: Frog Books; 1999.
Sheehan D, Moran C, Shanahan F (2015). The microbiota in inflammatory bowel disease. J Gastroenterol, 50(5):495- 507.
Singh S, Fatima Z, Hameed S (2016). Citronellal-induced disruption of membrane homeostasis in Candida albicans and attenuation of its virulence attributes. Rev Soc Bras Med Trop, 49(4):465-472.
Suzuki M, Hayama K, Takahashi M, Ezawa K, Yamazaki M, Matsukawa T, Kishi A, Satou N, Abe S (2015). The effects of aroma candy on oral Candida albicans colony- forming units (CFU) and oral hygiene states in healthy elderly carrying Candida albicans. Med Mycol J, 56(1):J31- 40. In Japanese.
Taguchi Y, Hayama K, Okada M, Sagawa T, Arai R, Abe S (2011). Therapeutic effects of cinnamaldehyde and potentiation of it efficacy in combination with methylcellulose on murine oral candidiasis. Med Mycol J, 52(2):145-152.
Takahashi M, Inoue S, Hayama K, Ninomiya K, Abe S (2012). Inhibition of Candida mycelia growth by a medium chain fatty acid, capric acid in vitro and its therapeutic efficacy in murine oral candidiasis. Med Mycol J, 53(4):255- 261. In Japanese.
Takakura N, Sato Y, Ishibashi H, Oshima H, Uchida K, Yamaguchi H, Abe S (2003). A novel murine model of oral candidiasis with local symptoms characteristic of oral thrush. Microbiol Immunol, 47:321-326.
Villanueva-Vilchis M-C, López-Ríos P, García I-M, Gaitán-Cepeda L-A. Impact of oral mucosa lesions on the quality of life related to oral health. An etiopathogenic study. Medicina Oral, Patología Oral y Cirugía Bucal. 2016; 21(2):e178-e184. doi:10.4317/medoral.20866.

LIMITED-TIME DEAL: ChatGPT PLUS/PRO at the LOWEST PRICE online!
GRAB YOUR SUBSCRIPTION NOW: ❣️ [url=https://bit.ly/UNLOCK-ChatGPT-PRO]ChatGPT PLUS/PRO[/url] ❣️
✅ WHY CHOOSE US?
✔ Instant activation – No waiting!
✔ Official subscription – No risk of bans!
✔ Cheaper than OpenAI’s website!
✔ Thousands of happy customers & 5-star reviews!
✔ 24/7 support – We’re here to help!
✅ HOW TO ORDER? (FAST & EASY!)
1️⃣ Click the link & select your plan.
2️⃣ Pay securely (Crypto, PayPal, Cards, etc.).
3️⃣ Receive your login OR unique activation code instantly!
4️⃣ Enjoy ChatGPT PLUS/PRO in minutes!
✅ WHAT’S INCLUDED?
⭐ GPT-4o (Fastest & Smartest AI!)
⭐ GPT-4 Turbo (Longer, detailed answers!)
⭐ Advanced AI features (Code Interpreter, Plugins, File Uploads!)
⭐ Priority access – No more downtime!
⚠ DON’T PAY FULL PRICE! Get ChatGPT PRO cheaper HERE:
❣️ [url=https://bit.ly/UNLOCK-ChatGPT-PRO]ChatGPT PLUS/PRO[/url] ❣️
⏳ DEAL ENDS SOON! Prices are rising—CLAIM YOUR SPOT NOW!
Access detailed information about the Audemars Piguet Royal Oak Offshore 15710ST here , including pricing insights ranging from $34,566 to $36,200 for stainless steel models.
The 42mm timepiece features a robust design with selfwinding caliber and rugged aesthetics, crafted in titanium.
https://ap15710st.superpodium.com
Check secondary market data , where limited editions command premiums , alongside pre-owned listings from the 1970s.
Request real-time updates on availability, specifications, and investment returns , with price comparisons for informed decisions.
rtg9sk
b1z1ef
На данном сайте можно получить Telegram-бот “Глаз Бога”, позволяющий найти всю информацию о человеке по публичным данным.
Сервис работает по номеру телефона, используя актуальные базы онлайн. Через бота доступны бесплатный поиск и глубокий сбор по запросу.
Сервис обновлен на 2025 год и поддерживает мультимедийные данные. Сервис сможет проверить личность по госреестрам и покажет сведения за секунды.
https://glazboga.net/
Это инструмент — идеальное решение для проверки людей онлайн.